Infections

One cause for acute brain swelling is infection. The yellow-tan clouding of the meninges seen here is due to an exudate from acute meningitis. |

Here is another example of an acute meningitis from bacterial infection. The cerebrospinal fluid (CSF) in such cases typically has a low glucose, high protein, and many PMN's. A gram stain should be done to identify organisms.

| Microscopically, a gram stain reveals gram negative diplococci within a neutrophil, typical for Neisseria meningitidis. Gram stain and culture can be performed on cerebrospinal fluid obtained via lumbar puncture. A variety of bacteria can cause meningitis, but several are more common, and have an incidence more frequent at certain ages: |
| ORGANISM | PEAK AGE INCIDENCE | GRAM STAIN |
|---|---|---|
| Escherichia coli | Neonates | Gram negative rods |
| Hemophilus influenzae | Infants and Children | Gram negative coccobacilli |
| Neisseria meningitidis | Adolescents and Young adults | Gram negative diplococci |
| Streptococcus pneumoniae | Older adults or Children | Gram positive cocci in chains |

Disseminated infections can be seen in immunocompromised hosts. Such infections can include fungi. Seen here are branching hyphae of Aspergillus invading a cerebral vessel. Aspergillus likes to invade vessels and produce hemorrhage and thrombosis. |

This is a cerebral abscess. There is a liquefactive center with yellow pus surrounded by a thin wall. Abscesses usually result from hematogenous spread of bacterial infection, but may also occur from direct penetrating trauma or extension from adjacent infection in sinuses.

Note the marked dilation of the cerebral ventricles. This is hydrocephalus. Hydrocephalus can be due to lack of absorption of CSF or due to an obstruction to flow of CSF
_______________________________________________________________
Congenital Malformations

Anencephaly is absence of the fetal cranial vault. Exposure of cerebral tissue to amniotic fluid precludes brain development. Anencephaly is a form of neural tube defect that is typically an isolated birth defect that is not related to chromosomal abnormalities.

Microscopically, the "area cerebrovasculosa" from the base of the skull from an anencephalic consists of scattered primitive neuroglial tissue elements within an irregular vascular proliferation. |

This is holoprosencephaly in which there is a single large ventricle with fusion of midline structures, including thalami. The affected fetuses and neonates typically have severe facial defects, such as cyclopia, as well. Underlying chromosomal abnormalities, such as trisomy 13, or maternal diabetes mellitus are possible causes, but some cases are sporadic.

The skull is opened here to reveal the "semilobar" form of holoprosencephaly, because there is a small cleft representing an attempt to separate the hemispheres. There is no gyral pattern seen here (lissencephaly) because this stillborn fetus was under 20 weeks gestation. Holoprosencephaly is a grave condition with little or no brain function.

The skull is opened in this third trimester stillborn fetus to reveal hydranencephaly. In this condition, there is an intrauterine event, such as an arterial occlusion, which leads to extensive cerebral infarction, typically involving the hemispheres. All that is left is a thin rim of cortex or glial tissue with meninges surrounding a fluid-filled cavity. |
_________________________________________________________________
Acquired and Congenital Degenerative Diseases

Here is anterior vermian atrophy of the cerebellum in a patient with chronic alcoholism. |
The small petechial hemorrhages in the mammillary bodies seen here are characteristic for Wernicke's disease, another complication of chronic alcoholism with thiamine deficiency |
Seen here in white matter is a large "plaque" of demyelination. The plaque has a grey-tan appearance. Such plaques are typical for multiple sclerosis (MS). These plaques lead to the clinical appearance of transient or progressive loss of neurological function. Since the disease is multifocal and the lesions appear over time, the clinical findings can be quite varied.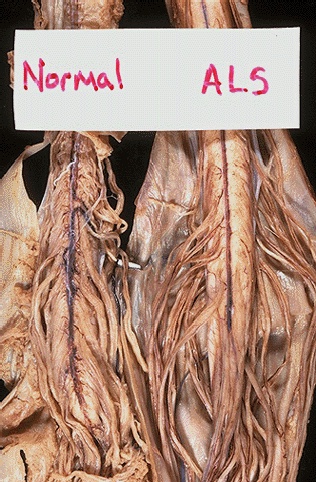 Amyotrophic lateral sclerosis (ALS) is uncommon. It begins in middle age and proceeds to death in several years. There is loss of anterior horn cells, so that patients present with progressive weakness that proceeds to paralysis from neurogenic muscular atrophy. Because of the loss of anterior horn cells, the anterior (ventral) spinal motor nerve roots demonstrate atrophy, as seen here in comparison withnormal ventral spinal cord nerve roots.  |

These enlarged, pale neurons are in a baby with Tay-Sachs disease, which is seen mostly in persons of European Jewish heritage. The disease is often first noticed at an age of 6 months, because the baby is not progressing developmentally.

This is an example of neuronophagia in which a dying neuron is surrounded by microglial cells.

| This is a so-called pseudolaminar necrosis of the cerebral cortex that is typical of a patient in a persistent vegetative state who is on life-support systems. Note that the cortical ribbon is very thin because of the loss of cortex. _____________________________________________________________ |
