CNS Hemorrhage

This is intraventricular hemorrhage (IVH) which arose in the subependymal region (germinal matrix) of a 28 week gestational age newborn. The germinal matrix region is very susceptible to such lesions at this period of development, leading to IVH as a complication of prematurity.

Hemorrhages involving the basal ganglia area (the putamen in particular) tend to be non-traumatic and caused by hypertension, which damages and weakens the small penetrating arteries. A mass effect with midline shift, often with secondary edema, may lead to herniation.

A blood clot is seen over the external surface of the dura. Thus, this is an epidural hematoma. Such a location for hemorrhage is virtually always the result of trauma that causes a tear in the middle meningeal artery.

The dura has been reflected back (with a small portion visible at the lower right) to reveal a subdural hematoma. Such a blood clot is usually the result of trauma with tearing of the bridging veins.

The dura has been reflected above to reveal the bridging veins that extend across to the superior aspect of the cerebral hemispheres. These can be torn with trauma, particularly if there is significant cerebral atrophy that exposes these veins even more.

Here is a bilateral chronic subdural hematoma. The blood clots are brown to tan because of organization. Since the bleeding is venous, subdurals can form more slowly and insidiously than clots from arterial hemorrhages. Subdurals are most common in the very young and the elderly.

| The cerebral arterial circulation at the base of the brain is diagrammed here. A berry aneurysm is diagrammed at the final bifurcation of the right internal carotid artery. The most common locations for berry aneurysms are in the region of the anterior communicating and anterior cerebral, at the trifurcation of the middle cerebral, and at the bifurcation of internal carotid with posterior communicating. Vertebral-basilar aneurysms comprise <10% of cases. Multiple aneurysms occur in about 20 to 30% of cases. |
| Abbr | Name of Artery | Distribution |
|---|---|---|
| ACA | Anterior Cerebral Artery | Supplies most medial portions of frontal lobes and superior medial parietal lobes |
| AComA | Anterior Communicating Artery | Connects the anterior cerebral arteries at their closest juncture |
| ICA | Internal Carotid Artery | Ascends through base of skull to give rise to the anterior and middle cerebral arteries, and connect with posterior half of circle of Willis via posterior communicating artery |
| MCA | Middle Cerebral Artery | Trifurcates into temporal, frontal, and parietal branches that supply most of the parenchyma of these lobes |
| PComA | Posterior Communicating Artery | Connects the anterior circle of Willis with the posterior cerebral artery of vertebral-basilar circulation posteriorly |
| PCA | Posterior Cerebral Artery | Supplies the occipital lobe and the inferior portion of temporal lobe. A branch supplies the choroid plexus. |
| SCA | Superior Cerebellar Artery | Supplies the dorsal cerebellum, pons, and midbrain |
| BA | Basilar Artery | Formed by the junction of the two vertebral arteries, it terminates as a bifurcation into the posterior cerebral arteries |
| AICA | Anterior Inferior Cerebellar Artery | Supplies the inferior cerebellum and portions of pons and medulla |
| VA | Vertebral Artery | The vertebrals emerge from the posterior base of skull and merge to form the basilar artery |
| PICA | Posterior Inferior Cerebellar Artery | Supplies the posterior cerebellum, choroid plexus in 4th ventricle, and portions of medulla |
| ASA | Anterior Spinal Artery | Descends along the anterior (ventral) aspect of the spinal cord |

The white arrow on the black card marks the site of a ruptured berry aneurysm in the circle of Willis. This is a major cause for subarachnoid hemorrhage.

The circle of Willis has been dissected, and three berry aneurysms are seen. Multiple aneurysms are seen in about 20-30% of cases of berry aneurysm. Such aneurysms are "congenital" in the sense that the defect in the arterial wall is present from birth, but the actual aneurysm takes years to develop, so that rupture is most likely to occur in young to middle age adults.

The subarachnoid hemorrhage from a ruptured aneurysm is more of an irritant producing vasospasm than a mass lesion.

Another cause for hemorrhage, particularly in persons aged 10 to 30, is a vascular malformation. Seen here is a mass of irregular, tortuous vessels over the left posterior parietal region.

The intraventricular and intracerebral hemorrhage seen here was due to a ruptured vascular malformation. The hemorrhage from such a lesion (which is most often histologically an arteriovenous malformation--AVM) can be intracerebral or extend into ventricles or subarachnoid space.

The microscopic appearance of this vascular malformation reveals the dilated, tortuous, worm-like vascular channels. Such lesions may bleed a small amount and be the cause for a seizure disorder.

The characteristic location of the hemorrhage in this brain is consistent with a fall backwards resulting in a contrecoup injury to the inferior frontal and temporal lobes. This has resulted in extensive contusions and subarachnoid hemorrhage.

The orange-brown, scalloped appearance of these lesions is consistent with old contusions. The resolution left behind hemosiderin from the hemorrhage that produces the orange-brown staining.

The lesions seen here are the result of extensive blunt force trauma to the head in a vehicular accident. Mainly the gyri are affected with hemorrhage from contusions and lacerations.

The so-called Duret hemorrhages seen here in the pons are secondary to downward compression that leads to stretching and ischemia of perforating arterioles. The compression can result from a variety of lesions--hemorrhages, edema, mass lesions of any type.
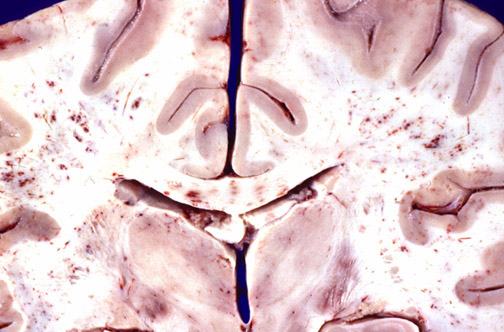
The extensive white matter petechial hemorrhages seen here are typical for fat embolism syndrome. Interestingly, neurologic signs and symptoms usually appear about a week after the initiating event, such as long bone fractures in a vehicular accident.
________________________________________________________________
Dementias

The cerebral atrophy seen here mainly in the frontal and parietal regions is characterized by narrowed gyri and widened sulci. The atrophy seen here was due to senile dementia of the Alzheimer's type (Alzheimer's disease).

The cortical atrophy leads to compensatory dilation of the cerebral ventricles known as "hydrocephalus ex vacuo"

The characteristic microscopic findings of Alzheimer's disease include "senile plaques" which are collections of degenerative presynaptic endings along with astrocytes and microglia. These plaques are best seen with a silver stain, as seen here in a case with many plaques of varying size.

This is a neurofibrillary "tangle" of Alzheimer's disease. The tangle appears as long pink filaments in the cytoplasm. They are composed of cytoskeletal intermediate filaments

The very marked frontotemporal atrophy seen here is due to another much less common type of dementia known as Pick's disease. |
The apparent enlargement of the ventricles seen here is due to atrophy of the head of the caudate from neuronal loss with Huntington's disease, an autosomal dominant condition characterized clinically by choreiform movements. |
Microscopically, the caudate nucleus in Huntington's disease demonstrates loss of neurons along with gliosis. The onset of this disease occurs in middle age. This disease results from an abnormal gene on chromosome 4 which codes for a protein containing increased trinucleotide repeat sequences. The greater the number of repeats, the earlier the onset of the disease. Spontanenous new mutations are uncommon. |
The loss of pigmentation in the substantia nigra of the midbrain at the left in a patient with Parkinson's disease is contrasted with a normal midbrain at the right. Parkinson's disease is marked clinically by a "pill-rolling" tremor at rest, mask-like facies, and cogwheel rigidity of limbs, among other findings. |

| At the left, an H and E stain demonstrates a rounded pink cytoplasmic Lewy body in a neuron of the cerebral cortex from a patient with diffuse Lewy body disease, which can be a cause for dementia. Lewy bodies can also be seen in substantia nigra with Parkinson's disease. An immunoperoxidase stain for ubiquitin, seen at the right, helps demonstrate the Lewy bodies more readily. _____________________________________________________________ |
