This is the external appearance of a normal heart.The epicardial surface is smooth and glistening.The amount of epicardial fat is usual.The left anterior descending coronary artery extends down from the aortic root to the apex.
The aortic valve shows three thin and delicate cusps. The coronary artery orifices can be seen just above.The endocardium is smooth, beneath which can be seen a red-brown myocardium. The aorta above the valve displays a smooth intima with no atherosclerosis.
This is the tricuspid valve. The leaflets and thin and delicate. Just like the mitral valve, the leaflets have thin chordae tendineae that attach the leaflet margins to the papillary muscles of the ventricular wall below.
This is a normal coronary artery. The lumen is large, without any narrowing by atheromatous plaque. The muscular arterial wall is of normal proportion.
This is the normal appearance of myocardial fibers in longitudinal section. Note the central nuclei and the syncytial arrangement of the fibers, some of which have pale pinkintercalated disks.
______________________________________________________________
Atherosclerotic Cardiovascular Disease
The coronary artery shown here has narrowing of the lumen due to build up of atherosclerotic plaque. Severe narrowing can lead to angina, ischemia, and infarction.
This section of coronary artery demonstrates remote thrombosis with recanalization to leave only two small, narrow channels.
There is a severe degree of narrowing in this coronary artery. It is "complex" in that there is a large area of calcification on the lower right, which appears bluish on this H&E stain. Complex atheroma have calcification, thrombosis, or hemorrhage. Such calcification would make coronary angioplasty difficult.
This distal portion of coronary artery shows significant narrowing. Such distal involvement is typical of severe coronary atherosclerosis, such as can appear with diabetes mellitus or familial hypercholesterolemia. This would make a coronary bypass operation difficult.
There is a pink to red recent thrombosis in this narrowed coronary artery. The open, needle-like spaces in the atheromatous plaque are cholesterol clefts.
This high magnification of the atheroma shows numerous foam cells and an occasional cholesterol cleft. A few dark blue inflammatory cells are scattered within the atheroma.
his is about as normal as an adult aorta in America gets. The faint reddish staining is from hemoglobin that leaked from RBC's following death. The surface is quite smooth, with only occasional faint small yellow lipid streaks visible.
These three aortas demonstrate mild, moderate, and severe atherosclerosis from bottom to top. At the bottom, the mild atherosclerosis shows only scattered lipid plaques. The aorta in the middle shows many more larger plaques. The severe atherosclerosis in the aorta at the top shows extensive ulceration in the plaques.
Here is an example of an atherosclerotic aneurysmof the aorta in which a large "bulge" appears just above the aortic bifurcation.Such aneurysms are prone to rupture when they reach about 6 to 7 cm in size. They may be felt on physical examination as a pulsatile mass in the abdomen.Most such aneurysms are conveniently located below the renal arteries so that surgical resection can be performed with placement of a dacron graft.
This microscopic cross section of the aorta shows a large overlying atheroma on the left. Cholesterol clefts are numerous in this atheroma. The surface on the far left shows ulceration and hemorrhage. Despite this ulceration, atheromatous emboli are rare (or at least, complications of them are rare).
This is a high magnification of the aortic atheroma with foam cells and cholesterol clefts
A coronary artery has been opened longitudinally. The coronary extends from left to right across the middle of the picture and is surrounded by epicardial fat. Increased epicardial fat correlates with increasing total body fat. There is a lot of fat here, suggesting one risk factor for atherosclerosis. This coronary shows only mild atherosclerosis, with only an occasional yellow-tan lipid plaque and no narrowing.
This is the left coronary artery from the aortic root on the left. Extending across the middle of the picture to the right is the anterior descending branch. This coronary shows severe atherosclerosis with extensive calcification. At the far right, there is an area of significant narrowing.
At high magnification, the dark red thrombus is apparent in the lumen of the coronary. The yellow tan plaques of atheroma narrow this coronary significantly, and the thrombus occludes it completely.
The anterior surface of the heart demonstrates an opened left anterior descending coronary artery.Within the lumen of the coronary can be seen a dark red recent coronary thrombosis. The dull red color to the myocardium as seen below the glistening epicardium to the lower right of the thrombus is consistent with underlying myocardial infarction.
Cross sections of this anterior descending coronary artery demonstrate marked atherosclerosis with narrowing. This is most pronounced at the left in the more proximal portion of this artery. In general, the worst atherosclerosis is proximal, where arterial blood flow is more turbulent. More focal lesions mean that angioplasty or bypass can be more useful procedures
Put down that jelly doughnut and look carefully at this aorta. The white arrow denotes the most prominent fatty streak in the photo, but there are other fatty streaks scattered over the aortic surface. Fatty streaks are the earliest lesions seen with atherosclerosis in arteries.
This is coronary atherosclerosis with the complication of hemorrhage into atheromatous plaque, seen here in the center of the photograph. Such hemorrhage acutely may narrow the arterial lumen.
A thrombosis of a coronary artery is shown here in cross section. This acute thrombosis diminishes blood flow and leads to ischemia and/or infarction, marked clinically by the sudden onset of chest pain.
Despite the frequency of aortic atherosclerosis, cholesterol emboli are rare, or at least insignficant most of the time. Seen here in a renal artery branch are cholesterol clefts of such an embolus. This patient had severe ulcerative, friable atheromatous plaques and had undergone angiography, which increases the risk for such emboli.
This is severe atherosclerosis of the aorta in which the atheromatous plaques have undergone ulceration along with formation of overlying mural thrombus.
________________________________________________________________
Myocardial Infarction
This is the left ventricular wall which has been sectioned lengthwise to reveal a large recent myocardial infarction. The center of the infarct contains necrotic muscle that appears yellow-tan. Surrounding this is a zone of red hyperemia. Remaining viable myocardium is reddish- brown.
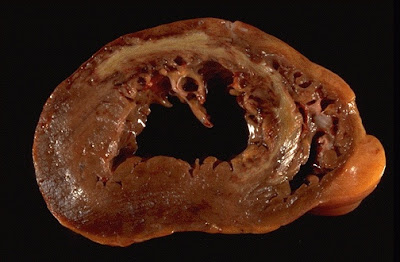
This cross section through the heart demonstrates the left ventricle on the left. Extending from the anterior portion and into the septum is a large recent myocardial infarction. The center is tan with surrounding hyperemia. The infarction is "transmural" in that it extends through the full thickness of the wall.
This high power microscopic view of the myocardium demonstrates an infarction of about 1 to 2 days in duration. The myocardial fibers have dark red contraction bands extending across them. The myocardial cell nuclei have almost all disappeared. There is beginning acute inflammation. Clinically, such an acute myocardial infarction is marked by changes in the electrocardiogram and by a rise in the MB fraction of creatine kinase.
In this microscopic view of a recent myocardial infarction, there is extensive hemorrhage along with myocardial fiber necrosis with contraction bands and loss of nuclei.
| This myocardial infarction is about 3 to 4 days old. There is an extensive acute inflammatory cell infiltrate and the myocardial fibers are so necrotic that the outlines of them are only barely visible. |
There is pale white collagen within the interstitium between myocardial fibers. This represents an area of remote infarction
The myocardium beneath the endocardial surface at the top demonstrates pale fibrosis with collagenization following healing of a subendocardial myocardial infarction.
The heart is opened to reveal the left ventricular free wall on the right and the septum in the center. There has been a remote myocardial infarction that extensively involved the anterior left ventricular free wall and septum. The white appearance of the endocardial surface indicates the extensive scarring.
There has been a previous extensive transmural myocardial infarction involving the free wall of the left ventricle. Note that the thickness of the myocardial wall is normal superiorly, but inferiorly is only a thin fibrous wall. The infarction was so extensive that, after healing, the ventricular wall was replaced by a thin band of collagen, forming an aneurysm. Such an aneurysm represents non-contractile tissue that reduces stroke volume and strains the remaining myocardium. The stasis of blood in the aneurysm predisposes to mural thrombosis.
One complication of a transmural myocardial infarction is rupture of the myocardium. This is most likely to occur in the first week between 3 to 5 days following the initial event, when the myocardium is the softest. The white arrow marks the point of rupture in this anterior-inferior myocardial infarction of the left ventricular free wall and septum. Note the dark red blood clot forming the hemopericardium. The hemopericardium can lead to tamponade.
n cross section, the point of rupture of the myocardium is shown with the arrow. In this case, there was a previous myocardial infarction 3 weeks before, and another myocardial infarction occurred, rupturing through the already thin ventricular wall 3 days later.
This patient underwent coronary artery bypass grafting with autogenous vein (saphenous vein) grafts. The largest of these runs down the center of the heart to anastomose with the left anterior descending artery distally. Another graft extends in a "Y" fashion just to the right of this to branches of the circumflex artery. A white temporary pacing wire extends from the mid left surface.
The earliest change histologically seen with acute myocardial infarction in the first day is contraction band necrosis. The myocardial fibers are beginning to lose cross striations and the nuclei are not clearly visible in most of the cells seen here. Note the many irregular darker pink wavy contraction bands extending across the fibers.
A cross section through the heart reveals a ventricular aneurysm with a very thin wall at the arrow. Note how the aneurysm bulges out. The stasis in this aneurysm allows mural thrombus, which is present here, to form within the aneurysm.
________________________________________________________________
Arterial Dissection
This microscopic cross section of the aorta demonstrates a red blood clot that is compressing the aortic lumen. This occurred as a result of aortic dissection in which there was a tear in the intima followed by dissection of blood at high pressure out through the muscular wall to the adventitia. This blood dissecting out can lead to sudden death from hemothorax.
Here, the dissection went into the muscular wall. In any case, an aortic dissection is an extreme emergency and can lead to death in a matter of minutes. The blood can dissect up or down the aorta. Blood dissecting up around the great vessels can close off the carotids. Blood can dissect down to the coronaries and shut them off.
This aorta has been opened longitudinally to reveal an area of fairly limited dissection that is organizing. The red-brown thrombus can be seen in on both sides of the section as it extends around the aorta. The intimal tear would have been at the left. This creates a "double lumen" to the aorta. This aorta shows severe atherosclerosis which, along with cystic medial necrosis and hypertension, is a risk factor for dissection.
This aortic dissection occurred just above the aortic root in a patient with Marfan's syndrome. The tear extends across the aorta. Hemopericardium with tamponade occurred within minutes of this event.
he mitral valve is shown in the same patient with Marfan's syndrome. The leaftlets of the mitral valve are redundant, and the one on the far left is ballooned upward. This is characteristic of floppy mitral valve with mitral valve prolapse. The chordae tendineae that hold the leaflets become long and thin. The characteristic finding on physical exam is a mid-systolic click.
This view of the mitral valve in a patient with Marfan's syndrome depicts a floppy mitral valve. The leaflet on the lower left has ballooned upward and the prolapse has resulted in contusion of the top of the leaflet, with a red black area of discoloration.
This mucin stain of the wall of the aorta demonstrates cystic medial necrosis, typical for Marfan's syndrome and causes the connective tissue weakness that explains the aortic dissection. Pink elastic fibers, instead of running in parallel arrays, are disrupted by pools of blue mucinous ground substance.
Microscopically, the tear (arrow) in this aorta extends through the media, but blood also dissects along the media (asterisk).
n aortic dissection may lead to hemopericardium when blood dissects through the media proximally. Such a massive amount of hemorrhage can lead to cardiac tamponade.
There is a tear (arrow) located 7 cm above the aortic valve and proximal to the great vessels in this aorta with marked atherosclerosis. This is an aortic dissection.
The right carotid artery is compressed by blood dissecting upward from a tear with aortic dissection. Blood may also dissect to coronary arteries. Thus patients with aortic dissection may have symptoms of severe chest pain (for distal dissection) or may present with findings that suggest a stroke (with carotid dissection) or myocardial ischemia (with coronary dissection).
_______________________________________________________________
Infective Endocarditis
| Here, infective endocarditis on the mitral valve has spread into the septum all the way to the tricuspid valve, producing a fistula. |
This is infective endocarditis. The aortic valve demonstrates a large, irregular, reddish tan vegetation.Virulent organisms, such as Staphylococcus aureus, produce an "acute" bacterial endocarditis, while some organisms such as Streptococcus viridans produce a "subacute" bacterial endocarditis.
The more virulent bacteria causing the acute bacterial form of infective endocarditis can lead to serious destruction, as shown here in the aortic valve. Irregular reddish tan vegetations overlie valve cusps that are being destroyed. Portions of the vegetation can break off and become septic emboli.
n this case, the infective endocarditis demonstrates how the infection tends to spread from the valve surface. Here, vegetations can be seen on the endocardial surfaces, and the infection is extending into to underlying myocardium.
Microscopically, the valve in infective endocarditis demonstrates friable vegetations of fibrin and platelets (pink) mixed with inflammatory cells and bacterial colonies (blue). The friability explains how portions of the vegetation can break off and embolize.
Here is a valve with infective endocarditis. The blue bacterial colonies on the lower left are extending into the pink connective tissue of the valve. Valves are relatively avascular, so high dose antibiotic therapy is needed to eradicate the infection.
Seen here in the finger at the right are small splinter hemorrhages in a patient with infective endocarditis. These hemorrhages are subungual, linear, dark red streaks. Similar hemorrhages can also appear with trauma.
Another small linear splinter hemorrhage is seen here subungually on the left thumb of a patient with infective endocarditis and blood culture positive for Staphylococcus aureus.